Last updated November 2024

A human foot has 26 bones, 33 joints, and more than 100 tendons, muscles, and ligaments. This complex structure not only gets us from here to wherever, but does so while supporting all our body weight. No wonder that 77 percent of Americans say they have experienced foot or ankle pain—from blisters and bunions to sprains, strains, and plantar fasciitis.
If you are suffering from foot or ankle problems, “it is important to see a podiatrist to establish a definitive diagnosis,” said J. John Hoy, a Seattle-based podiatrist. “Improper movement or exercise when immobilization is needed can make the condition worse.”
Here’s what podiatrists do, how to find one, and how to work with one.
What’s a Podiatrist?
There are more than 18,000 practicing podiatrists in the U.S. Also known as doctors of podiatric medicine (DPMs), these professionals are trained to diagnose and treat conditions of the foot and ankle. These include injuries, deformities, infections, and chronic conditions like arthritis or diabetes-related complications.
Podiatrists are doctors, but they’re not physicians. After earning a bachelor’s degree, podiatrists attend a four-year podiatric medical school to earn a DPM degree. They then complete a two- to three-year residency and must pass both the multi-part American Podiatric Medical Licensing Exam and state licensure tests.
DPMs can then pursue board certification in specialties such as foot and ankle surgery through the American Board of Podiatric Medicine (ABPM) and the American Board of Foot and Ankle Surgery (ABFAS). Some podiatrists also specialize further, in fields such as sports medicine or diabetic foot care.
The American Podiatric Medical Association (APMA), the professional organization for DPMs, represents about 80 percent of U.S. DPMs and provides educational programs to help its members maintain current licensure requirements.

What Do Podiatrists Do?
Podiatrists treat a wide range of foot and ankle issues, including ingrown toenails, warts, corns, and broken or sprained bones. They also address foot complications from diabetes, such as nerve damage and ulcers. Podiatric procedures range from simple (trimming callouses) to complex (bunion correction surgery).
Podiatrists often advise patients on footwear adjustments or fit custom orthotics to help alleviate lower extremity discomfort. For example, they might recommend shoes with wider toe boxes to relieve pressure on bunions or prescribe custom orthotics to correct balance and gait issues. Orthotics are often the first line of defense when a patient has flat feet, plantar fasciitis, overpronation, or bunions.
Many podiatrists also perform foot and ankle surgeries, including procedures to correct hammer toes, relieve plantar fasciitis, and bunionectomies. Most do minimally invasive surgeries (MIS), and refer patients to orthopedic surgeons for conditions which require extensive intervention.
When Is an Orthopedic Surgeon Necessary?
If your pain or injury involves other parts of the body besides your feet, an orthopedic surgeon might be a better choice. Orthopedists can address complex fractures, tendon or ligament repair, or joint replacements.
Anthony Ndu, an orthopedic surgeon at Penn Medicine in Philadelphia, said that while podiatrists can treat bunions or hammertoes, procedures such as mid- or hind-foot reconstructions or flat foot corrections are usually done by orthopedists.
Who Should See a Podiatrist?
“Even if you are feeling minor foot or ankle pain, you may need professional treatment to ensure that things heal properly,” said Joseph E. Mechanik, a podiatrist in Centennial, Colorado.
You may want to see a podiatrist if you are suffering from:
- Persistent foot or ankle pain that doesn’t improve with rest or over-the-counter pain medication.
- Injuries including strains, sprains, fractures, or dislocations.
- Changes in foot appearance including structural deformities (bunions, hammertoes); persistent redness or swelling (which could indicate infection); or skin changes including blisters, calluses or corns that don’t go away.
- Nail problems such as ingrown toenails or fungal infections. Many podiatrists offer medical pedicures (aka a “medi-pedi”) to treat minor ailments like ingrown nails, calluses, or fungal infections, or to help diabetics who require ongoing foot care. Insurance may cover a medical pedicure if it’s done by a board-certified podiatrist and billed correctly. Check with your insurance plan to find out if it will cover this as a medical pedicure. You can also use money in your flexible spending or health savings account (FSA or HSA) to pay for it.
- Diabetes: Consistent foot care can prevent serious complications like infections, neuropathy, and foot ulcers (open wounds that won’t heal). “If you have diabetes, regular visits are essential, even if you’re not experiencing symptoms,” said Hoy. “Any non-healing wounds or sores on your feet should be treated by a podiatrist.”
- Persistent foot odor, which could signal an infection.
- Difficulty walking, which may result in frequent falls. “When your feet are not properly aligned, it can greatly affect your balance,” said Mechanik. “Every step we take depends on the precise coordination of numerous ligaments, tendons and muscles.”
- Numbness or tingling in the feet or ankles, which could be the result of nerve damage or circulation problems.
Who Treats Bunions?
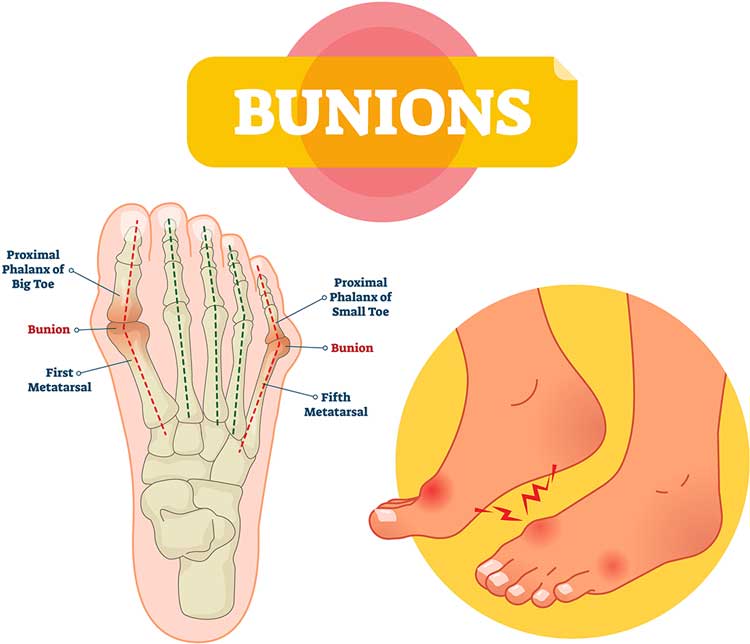
A bunion is a chronic dislocation of the big toe joint, often caused by long-term stress on its joint capsule (the first metatarsophalangeal joint). This makes the big toe angle toward the other toes, creating a bony bump on the side of the foot.
Both podiatrists and orthopedic surgeons can perform bunion surgeries (aka bunionectomies), which realign the bones and correct the deformity. Podiatrists tend to opt for less invasive treatments before surgery, such as pain medication, physical therapy, or orthotics. If you are unsure about the severity of your bunion, consulting a podiatrist is a good first step.
While podiatrists focus specifically on the structure of the foot and ankle, orthopedists study how these areas connect to the rest of the body. Have an advanced bunion which is impacting your legs, hips, or spine—or your gait, balance, and overall mobility? See an orthopedist.
Which Bunion Surgery—and Surgeon—Is Right for Me?
There are several types of bunion surgeries. The two most prevalent are the minimally invasive Chevron Akin and the more advanced Lapidus Procedure. Either can be performed by a podiatrist or orthopedist.
For the Chevron Akin, the doctor makes small incisions in the foot bones, inserting screws or pins to realign the big toe joint. Recovery time is usually six to eight weeks.
With the Lapidus, the doctor fuses the joint at the base of the big toe and first metatarsal bone. This involves cutting into bone, removing cartilage, and using screws or plates to hold bones in place while they heal. The recovery period is longer—up to three months for the bones to heal and another nine months for swelling to subside.
Which procedure is right for you? It depends on the severity of your condition and on whether the podiatrist or orthopedist thinks the bunion will reoccur. In general, more serious issues require more invasive surgery. But, Hoy warned that: “There are far too many doctors who recommend the Lapidus for treating all bunions.” Get several opinions, and consult both kinds of doctors.
How Do You Find a Great Podiatrist?
Ask friends and family for suggestions. Here at Checkbook.org, you’ll find reviews and recommendations of local practices.
Most health insurance plans cover podiatric care at some level. Before making an appointment, confirm that the practice accepts your coverage, and ask your insurer whether you need a referral from your primary care physician.
What Should You Do Before Going to a Podiatrist?
Write up notes about your symptoms. When did problems start, or when did the injury occur? Was there swelling, numbness, increasing pain, etc.? What have you done to treat them?
Be ready to discuss your medical history, including other medical conditions and medications you take. Also, bring any past medical records, including X-rays that document treatments or surgeries of your foot and ankle.
Make a list of all questions you want to ask your podiatrist so you don’t forget anything. Take notes!
Personal hygiene counts. Clean your feet and avoid using any creams or lotions on the day of your podiatry visit. Remove nail polish if your condition involves your toenails so the doc can get a better look at what’s going on.


